Author: Sandhya Chandrasekaran (MP2)
The East Harlem Health Outreach Partnership (EHHOP), Mount Sinai’s student-run free clinic, has been serving uninsured patients in the East Harlem area for 12 years. Since its inception in 2004, EHHOP has steadily evolved from an urgent care model into the primary care home for over 200 patients. This growth has largely been due to the indispensable synergy of preceptor mentorship and student involvement. And as MD/PhDs committed to a dual-degree program, we are in the unique position to both contribute to and benefit from EHHOP in several fundamental ways over the duration of our training.
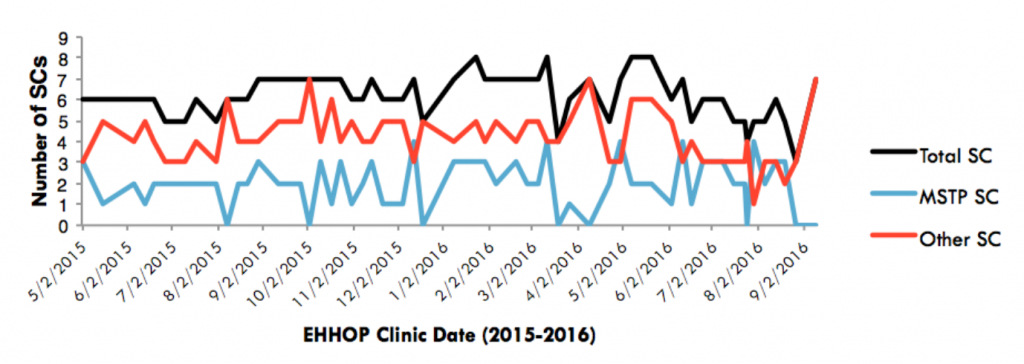
The number of total senior clinicians (SCs, black) at EHHOP must remain close to 7 to comfortably accommodate the number of patients scheduled for Saturday clinic. While third- and fourth-year MD students generally volunteer very regularly (red), MSTPs in their PhD+ phase (blue) volunteer regularly as well, roughly compensating for major dips in the senior clinician pool due to medical student scheduling conflicts. In recent months, MSTPs have been increasing their volunteering commitments — hopefully, a trend that persists in the coming years!
On Saturday clinic days at EHHOP, a junior clinician (first or second year medical student) assists a senior clinician (third or fourth year medical student, or an MD PhD student in the PhD+ phase) who serves as the predominant medical interviewer. The history and physical examination information jointly gathered from the encounter by these students is then discussed with an attending preceptor to finalize an assessment and plan. For MD/PhDs in their PhD phase, this system not only offers a venue for regular note writing and oral presentation practice, but also provides ample opportunities for teaching students and developing mentorship qualities.
Clearly, EHHOP’s inherent structure relies heavily on senior clinician involvement to address patients’ medical concerns. However, given that many of these senior clinicians are third- and fourth- year medical students balancing demanding clerkships, shelf exams and residency interviews, certain weekends conceivably suffer from lower volunteer commitment. As the PhD years offer more flexibility with respect to specific work hours, MD/PhD students are prime substitutes. Indeed, MD/PhD involvement has reliably compensated for fluctuations in medical student involvement over the course of the last year to keep overall senior clinician numbers relatively stable year round, especially considering the size of our program in relation to the third- and fourth- year medical school classes.
Our additional years as practicing senior clinicians also afford us the opportunity to follow select patients longitudinally, consequently forging deep bonds and meaningful connections with some of the clinic’s sickest and medically complex patients. Jennifer Diaz, a sixth year in the program, has been following one of her patients for three years now, having honed her skills in hemodialysis and blood pressure management as a result. She attests, “I think patients have a lot to teach, and following them longitudinally gives us space to really learn from them. Each patient is unique. Given time, you learn to utilize clinical reasoning that incorporates your previous experience with the patient and the latest clinical research, rather than blindly applying textbook knowledge.” This chronic care dynamic builds upon the concept of ‘longitudinal clinical exposure’ or LCE introduced in the preclinical medical curriculum by granting MD/PhD students the responsibilities of overseeing patient care firsthand.
Understandably, years removed from regular clinical exposure renders MD/PhD students in their PhD phase both unconfident about their medical competence and anxious about their integration into third year rotations. To this end, Dr. Yasmin Meah and Robert Rifkin, a current seventh year in the program, meticulously designed and launched the EHHOP Clinical Service Enrichment Program (CSEP) for MD/PhDs in 2014, with the goal of providing concrete medical milestones and a structured platform for critical clinical practice discussions. Under the guidance of Benjamin Laitman and Noa Simchoni, the program has since morphed into tailored didactic sessions from physician experts; CSEP has received overwhelmingly positive reviews from students since it began.
Arguably, fueling EHHOP’s continued progress is its investment in research. MD/ PhDs have been instrumental in this effort by organizing and heading the EHHOP Quality Improvement Council (QIC). Now in its sixth year, the QIC caters to the budding research interests of preclinical students by equipping them with the tools to critically analyze and address key issues within EHHOP’s infrastructure in several successive ‘plan-dostudy-act’ (PDSA) cycles. Naturally, the QIC appeals to the research-oriented minds of MD/ PhD students, and has indeed benefitted from strong MD/PhD participation and leadership in coordinating QIC projects and initiatives.
With so many opportunities for involvement, it comes as no surprise that MD/PhDs have percolated several roles on the steering and executive leadership committees of EHHOP – overseeing research, finance, technology, education, and pharmacy. As such, it is clear that our steady presence in these capacities affords the clinic the necessary glue to hold together multiple isolated medical encounters in the context of a free clinic striving to better suit the needs of the patient population it strives to serve.
